Reflecting on a remarkable journey over seven transformational years
My name is Catherine Pickering and I’m the Co-Founder and CEO of iOnctura, a clinical-stage biopharmaceutical company combating neglected and hard-to-treat cancers.
When you are a CEO of a thriving, fast-moving company you rarely have a moment to reminisce over the journey you have been on. Today, on the back of our Series B announcement I am excited to have the opportunity to do that.
A successful finance round, especially after navigating through a few years of external financing turmoil, brings excitement and a renewed energy to push forward to fulfil all of those plans you have been selling for the months leading up. It is a special moment to be able to look backwards over the years and consider the journey that you’ve been on and those people who were with you.
My personal journey started in 2017 when I headed up the Global Oncology Licensing team at Merck. I decided that I wanted to build my own company that focussed on cancer types that remained neglected and under-researched with a portfolio of early stage molecules that I had hunted down with the help of colleagues and collaborators. After reaching out to a few friendly investors who guided me on what they would need to see to invest, six months of heavy licensing and investment negotiations, some 101 company creation lessons and convincing MVentures to invest, iOnctura was born seven years ago this month.


In those early formation days, we didn’t have money to spend on branding or communications so my Co-Founder Lars van der Veen and I put our heads together and came up with a word that described the mission.
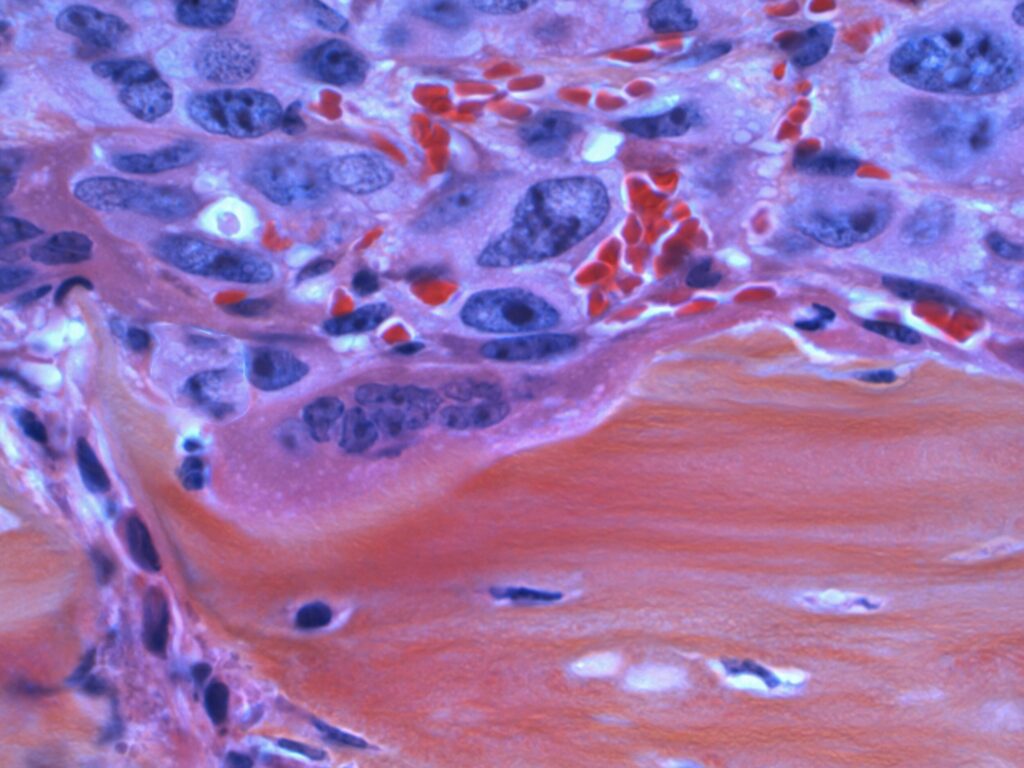
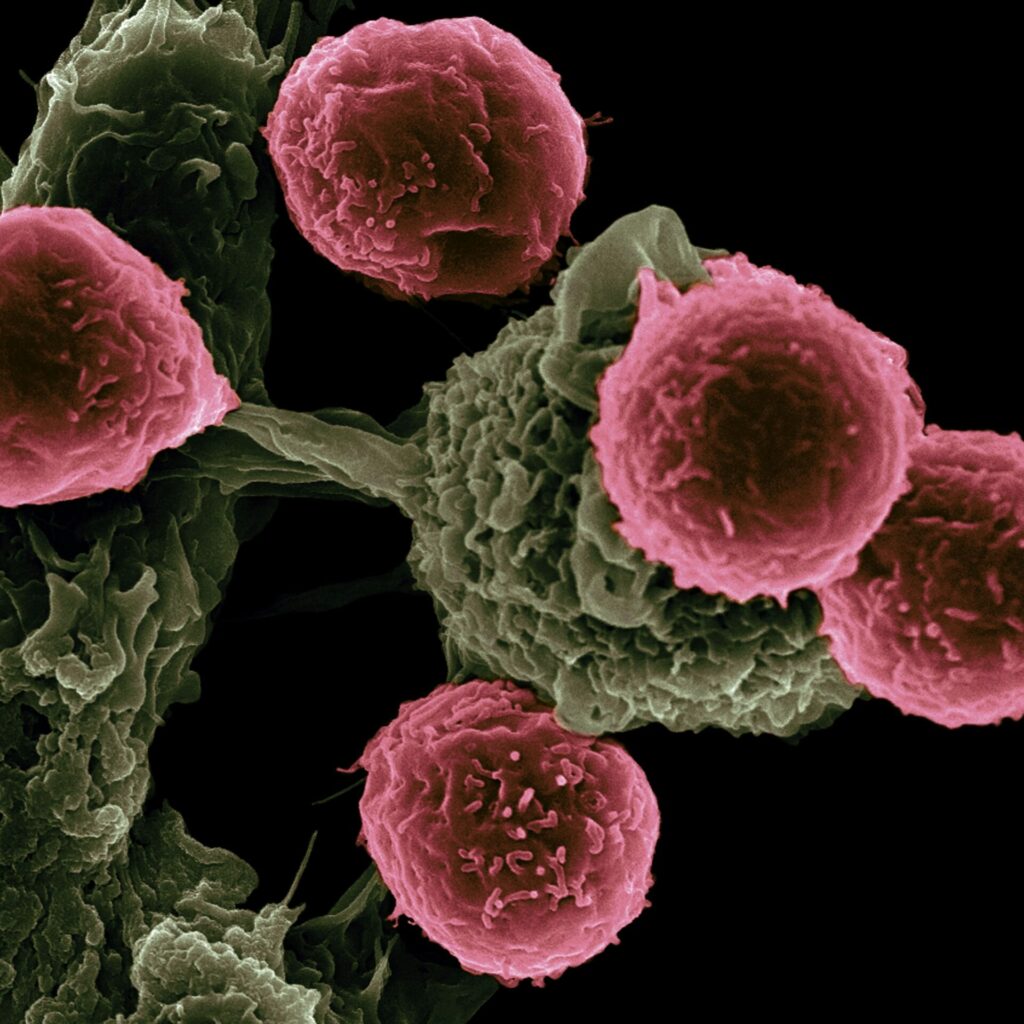
Many people ask where the name iOnctura comes from. In those early formation days, we didn’t have money to spend on branding or communications so my Co-Founder Lars van der Veen and I put our heads together and came up with a word that described the mission of iOnctura which was, and still is, combining safe and effective drugs to precision inhibit parallel tumor survival mechanisms (iūnctūra; meaning a joining, uniting; an association).
The journey has certainly been exhilarating… We have built the company from one employee to now over 20, entered many academic collaborations worldwide with world renowned researchers and investigators, and expanded our pipeline to build a strong precision-focussed portfolio. We have raised nearly 130m in dilutive and non dilutive financing and are on the cusp of taking our two lead clinical program into multiple Phase two studies.
The future is looking very exciting for iOnctura as we move into a phase where we are close to being able to bring a treatment, and along with it hope, to patients suffering from a rare condition of the eye. We expect to continue to demonstrate positive and long lasting impact of roginolisib in UM and other subsequent cancer types without disrupting the quality of those moments left for patients to spend with their families.
iOnctura would not be the success it is today without the team. So perhaps we can also use the meaning of ionctura — joining, uniting — to describe the people who have made this journey a success a story. I would like to thank each and every one of the iOnctura team (especially my Co-Founder Lars van der Veen), my patient, courageous and nurturing investors (new and existing) and last but by no means least my gorgeous family.
Here’s to seeing what the next seven years bring!